DNA methylation changes in neurons of bipolar disorder patients
 CC by 4.0" width="800" height="479">
CC by 4.0" width="800" height="479">
A research collaboration based in Kumamoto University, Japan, has revealed the DNA methylation status of gene transcriptional regulatory regions in the frontal lobes of patients with bipolar disorder (BD). The regions with altered DNA methylation status were significantly enriched in genomic regions which were reported to be genetically related to BD. These findings are expected to advance the understanding of the pathogenesis of BD and the development of therapeutic drugs targeting epigenetic conditions.
BD is amental disorderthat affects about 1% of the population and requires long-term treatment. Epidemiological studies have suggested that the onset of the disease is related to a complex interaction of genetic and environmental factors. Epigenetic changes in the genome, particularly in the repression of gene expression through DNA methylation, are thought to be deeply involved in the pathogenesis of various diseases, including mental disorders.
Previous studies analyzed DNA methylation using peripheral blood and saliva samples to identify genes with altered DNA methylation and use them as biomarkers. Since mental disorders are diseases of the nervous system, research usingbrain tissueis particularly important. However, in addition to the scarcity of samples, brain tissue is a mixture of various cell types, such as neurons and glial cells, and is affected by differences in the ratio of cell types contained in the tissue, making accurate analysis difficult.
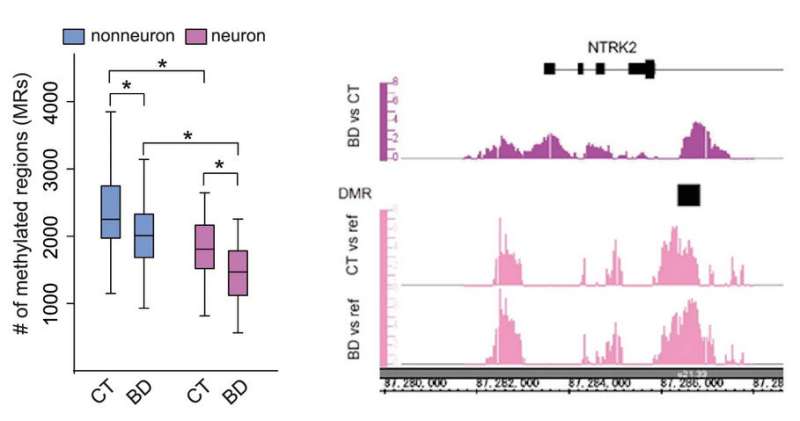
The researchers used neuronal nuclear markers to fractionate frontal lobe samples from 34 BD patients and 35 healthy subjects into neuronal and non-neuronal cell nuclei. Genomic DNA extracted from each of these samples was then used to examine the DNA methylation status of the regulatory regions of gene transcription using an array method. They found that many genes in both neurons and non-neurons were hypomethylated in BD patients compared to healthy subjects. On the other hand, genes important for psychiatric and neurological functions were found to be hypermethylated in neurons.
To investigate the effects of mood stabilizers—drugs used to treat BD—the researchers cultured human neuroblastoma cells in the presence of mood stabilizers (lithium, valproate and carbamazepine) in effective blood concentration ranges and measured DNA methylation status. They found that about 30% of the regions with altered DNA methylation status in BD patients overlapped with mood stabilizers-induced DNA methylation changes. Most of the DNA methylation changes were in the opposite direction of those in the postmortem brain, which the researchers thought reflected the effects of the treatment. They also measured the expression levels of 10 genes associated with DNA methylation changes and found that the DNMT3B gene, a DNA methyltransferase, was elevated in BD patients, suggesting that it may be associated with neuron-specific DNA methylation changes.
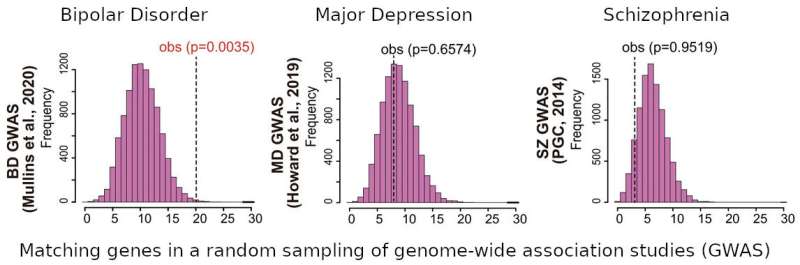
Finally, the researchers compared thegenomic regionsassociated with mental disorders as identified ingenome-wide association studies(GWAS) with regions having an altered DNA methylation status. Significant accumulation was observed in the genomic regions reported in the GWAS for BD, while no accumulation was observed in the genomic regions reported for depression and schizophrenia.
"The clarification of neuron-specific DNA methylation changes and characteristics is expected to greatly advance our understanding of the pathogenesis ofbipolar disorder," said Professor Kazuya Iwamoto, who led this study. "We also expect that this will help in the development of therapeutic drugs targeting epigenetic conditions."





















