This article has been reviewed according to Science X'seditorial process一个ndpolicies.Editorshave highlighted the following attributes while ensuring the content's credibility:
fact-checked
peer-reviewed publication
trusted source
proofread
Blood pressure medication combined with chemotherapy could reduce spread in triple negative breast cancer
A new international study led by Monash University has, for the first time, identified that beta-blockers could significantly enhance the therapeutic effect of anthracycline chemotherapy in triple negative breast cancer (TNBC) by reducing metastasis.
Anthracyclines are a class of drugs used in chemotherapy to treat many cancers, including TNBC.
Researchers from the Monash Institute of Pharmaceutical Sciences (MIPS) have previously shown in a clinical trial that beta-blockers (most commonly used to manageblood pressure) are linked with less cancer spread. However, until now, it was unclear how beta-blockers would interact with common cancer treatments.
In this new study, published inScience Translational Medicine, the MIPS team used mouse models of cancer and analyzed large-scale patient clinical data, in collaboration with the Cancer Registry of Norway, to discover that anthracycline chemotherapy on its own, in the absence of a beta-blocker, induces nerve growth in tumors.
However, adding a beta-blocker to chemotherapy inhibited nerve fiber activity in tumors and stopped the cancer from coming back after treatment.
MIPS Research Fellow and the study's lead author, Dr. Aeson Chang, said the findings reveal an unanticipated insight into why chemotherapy treatment does not always work as it should.
"We set out to build on previous studies that have shown beta-blockers can halt thestress responseexperienced bycancer patients一个t the time of diagnosis and stop the cancer from spreading.
In this new study, not only did we discover the biological effect of beta-blockers when used alongside anthracycline chemotherapy, we also discovered why they are effective," said Dr. Chang.
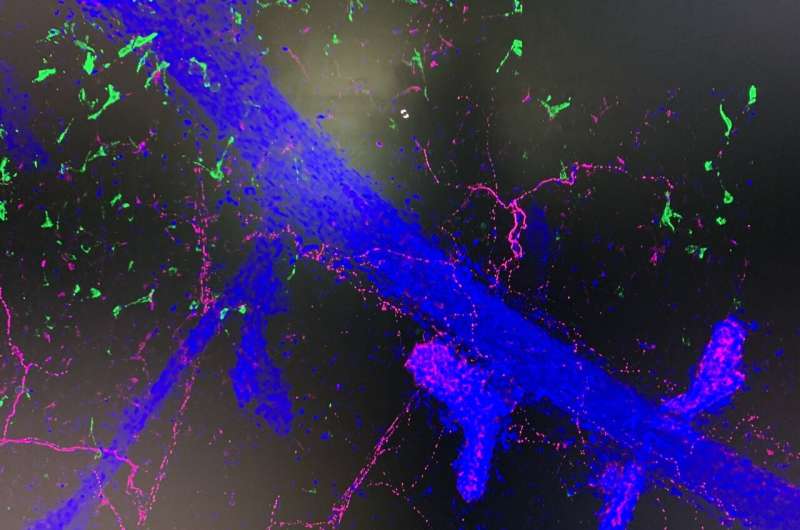
"In mouse models of TNBC, we found that anthracycline chemotherapy was able to increase sympathetic nerve fiber activity in tumors. Activation of these stress neurons can help tumor cells spread and, fortunately, we found that beta-blockers could stop this effect. Our hope is that this exciting discovery will pave the way for further research and, ultimately, lead to improved outcomes for patients."
Senior author, Professor Erica Sloan, who has been exploring the use of beta-blockers as a novel strategy to slow cancer progression for a number of years, said the study provides important clues about why beta-blockers may help improve the clinical management of TNBC.
"While many patients will be cured by treatment, unfortunately, in some patients the cancer may return—this study has helped us understand why. Our findings show that anthracycline chemotherapy supports the growth of nerves, which can support cancer relapse. This is important, as it tells us that targeting nerves using abeta-blockercan improve response to treatment," said Professor Sloan.
"Beta-blocker use has been consistently linked to reduced metastatic relapse and cancer-specific survival in TNBC patients. However, the lack of understanding of how beta-blockers improvechemotherapy—which is a core component of the standard treatment for TNBC—has limited the translation of these findings into thecancerclinic," said Professor Sloan.
"We believe this study presents an exciting opportunity to further explore the use of beta-blockers as a novel strategy in thetreatmentof TNBC."
More information:Aeson Chang et al, Beta-blockade enhances anthracycline control of metastasis in triple-negative breast cancer,Science Translational Medicine(2023).DOI: 10.1126/scitranslmed.adf1147


















