This article has been reviewed according to Science X'seditorial processandpolicies.Editorshave highlighted the following attributes while ensuring the content's credibility:
fact-checked
trusted source
proofread
Study uncovers reduced exercise tolerance and other changes in 'long COVID'
A recent study published inPulmonary Circulationassesses changes in oxygen extraction following post-acute sequelae of SARS-Cov-2 infection (PASC) syndrome, or "long COVID." PASC may affect half of patients who recover from COVID-19. One debilitating hallmark is a persistent decrease in exercise tolerance.
This study, led by Inderjit Singh, MBChB, BMedSci, FRCP, assistant professor (pulmonary,critical care, and sleep medicine) and Hyung J. Chun, MD, associate professor adjunct (cardiovascular medicine), assessed a cohort of patients using invasive cardio-pulmonary exercise testing, which was conducted in parallel for each patient with multiplex proteomics profiling evaluating thousands of circulating proteins.
While prior studies have shown dysregulated alterations in theimmune systemfollowing COVID-19 infection, no study to date had associated such findings with the impaired oxygenextractionthat may be a critical driver of persistent exertional intolerance in long COVID patients.
"We previously demonstrated on invasive cardiopulmonary exercise testing (iCPET) that the pathophysiologic abnormality in patients with PASC was a primary peripheral limit to exercise characterized by impaired or systemic oxygen extraction," states Singh. "This current study combined our iCPET capability with an unbiased proteomic analysis to better understand why PASC patients experience this impaired oxygen extraction phenomenon."
Differences in cardiopulmonary responses to exercise
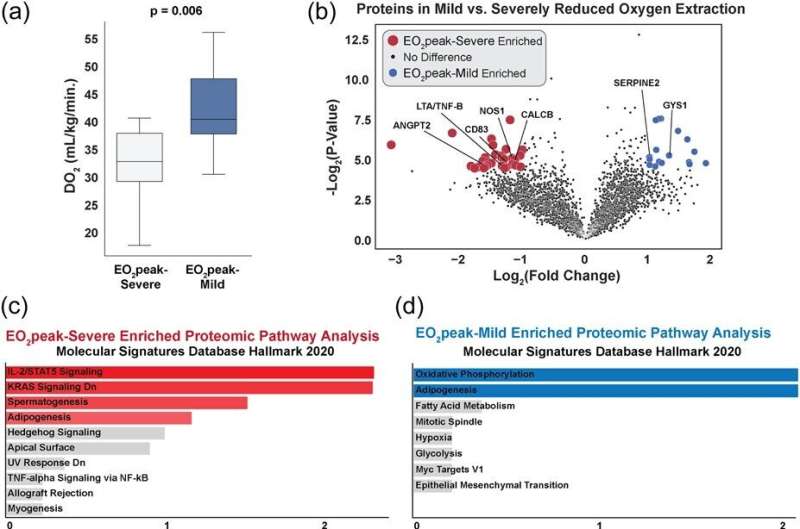
A large cohort of PASC patients referred to the Yale New Haven Hospital Pulmonary Vascular Disease Clinic with continued inability to partake inphysical activitytypically associated with their age underwent invasive cardiopulmonary testing. The authors identified two subsets of PASC patients: those with mild reduction in the body's ability to extract oxygen from the blood, and those with severe reduction in oxygen extraction capacity.
Multiomic proteomic analysis of blood collected from these patients identified increased circulating levels of proteins implicated in the inflammatory and fibrotic processes among the PASC patients with severely-reduced oxygen extraction capacity, as well as increased levels of proteins associated withendothelial dysfunction, or the inner layer of blood vessels critical for normal function of the lungs in extracting oxygen.
Singh states, "The current study shows that there exists a dichotomy of cardiopulmonary and proteomic phenotype that begets the observed impaired systemic oxygen extraction in PASC. These distinct cardiopulmonary proteomic phenotypes can help foster future studies to develop a personalized medicine approach for the different PASC phenotypes."
Chun adds, "These findings not only identify new mechanisms that may help identify those patients most likely to develop persistent long COVID symptoms, but also identify disease mechanisms that may be potentially targeted to improve the long COVID symptoms."
Overall, there is a continuum of biologic changes inoxygenextraction that may affect patients with PASC. Pathways related to inflammation and endothelial dysfunction may be implied, as the authors discuss.
Future work assessing biological mechanisms and functional pathways altered by such atypical protein expressions are necessary to improve therapies for those suffering from long COVID. Chun states, "At the moment, we still have no effective treatment for patients who continue to struggle with long COVID. We hope to apply our new findings to develop new treatment strategies that will need to be rigorously tested to see if they may offer benefit to the long COVID patients."
更多的信息:Inderjit Singh et al, Proteomic profiling demonstrates inflammatory and endotheliopathy signatures associated with impaired cardiopulmonary exercise hemodynamic profile in Post Acute Sequelae of SARS‐CoV‐2 infection (PASC) syndrome,Pulmonary Circulation(2023).DOI: 10.1002/pul2.12220





















